
Margin quality analysis for wedge resection of lung cancer and construction of a predictive model
Highlight box
Key findings
• By analyzing data of 530 patients who underwent pulmonary wedge resection for non-small cell lung cancer (NSCLC), we identified longer max distance to pleura and larger tumor size as risk factors associated with insufficient wedge resection margin. While preoperative localization and right-side surgery were protective factors for resection margin. A predictive model and the derived nomogram were built to preoperatively estimate the risk of an insufficient wedge resection margin for individual patient.
What is known and what is new?
• According to the National Comprehensive Cancer Network guideline for NSCLC, pulmonary wedge resection should achieve a parenchymal resection margin of more than 2 cm or the size of the nodule. Insufficient or guideline discordant resection margin is associated with malignant positive margins and high local recurrence risk. However, not all wedge resections achieve a satisfactory resection margin. And there is no study that investigates the current clinical status and risk factors of guideline discordant resection margin.
• We innovatively investigated the clinical characteristics of patients with guideline concordant or discordant wedge resection margin and developed a clinical model and the associated nomogram to preoperatively predict the risk of discordant margin.
What is the implication, and what should change now?
• Using our preoperative predictive model to estimate the risk of an insufficient wedge resection margin, preoperative localization or individualized surgical plans can be made for high-risk patients.
Introduction
With the wide application of computed tomography (CT) screening, the incidence of early-stage lung cancer has increased remarkably in recent years (1-3). Although lobectomy is a traditional and prevalent surgical treatment for resectable non-small cell lung cancer (NSCLC), sublobar resections, including wedge resection and segmentectomy, have been established as equally effective and safe, and are increasingly recognized as the standard of care for early-stage disease (4-6).
According to current clinical practice and the National Comprehensive Cancer Network (NCCN) Guideline for lung cancer (7,8), wedge resection is appropriate in patients with limited pulmonary function and other contraindications for lobectomy, or peripheral nodule less than 2 cm in diameter. Wedge resection should also achieve a parenchymal resection margin of more than 2 cm or the size of the nodule. Studies have indicated that insufficient or guideline discordant resection margin distance is significantly associated with malignant positive margins (9) and high local recurrence risk (10,11). However, not all wedge resections achieve a satisfactory resection margin (9,11). From a clinical point of view, tumor size, distance between tumor and pleura, surgical technique and even surgeon experience could probably affect the quality of the resection margin. However, there is no study which investigates the current clinical status and risk factors of guideline discordant resection margin.
In this study, we aim to first investigate the clinical characteristics of patients with guideline concordant or discordant wedge resection margin and develop a simple clinical model and the associated nomogram to preoperatively predict the risk of discordant margin. We present this article in accordance with the TRIPOD reporting checklist (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-22/rc).
Methods
Patients and data collection
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine (approval number 2023-15) and individual consent for this retrospective analysis was waived.
Patients who had pulmonary malignancies and underwent pulmonary wedge resection between April 2014 and February 2023 in the Department of Thoracic Surgery, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine were eligible for this retrospective study. The exclusion criteria were: (I) confirmed metastasis or benign lesion according to postoperative pathology; (II) tumor diameter >2 cm; (III) incomplete patient data (e.g., surgical margin, pulmonary function). Ultimately, 530 patients were included in this study.
Patients’ clinical data were retrospectively recorded from the lung cancer database of our department. Variables for each patient included sex, age, body mass index (BMI), percentage of the predicted value of forced expiratory volume in one second (%FEV1), the ratio of forced expiratory volume in one second and forced vital capacity (FEV1/FVC), percentage of the predicted value of maximal voluntary ventilation (%MVV), tumor’s minimal distance to pleura, max distance to pleura, tumor size, surgical margin distance, surgical type (wedge resection, wedge resection combined with lobectomy or segmentectomy), surgical technique (thoracotomy, video-assisted thoracic surgery, or robotic-assisted thoracic surgery), surgical location (upper lobe or not, left or right sided surgery), preoperative pulmonary nodule localization, history of lung disease (asthma, chronic bronchitis, etc.), history of cardiovascular disease (coronary heart disease, arrhythmia, heart valve disease, etc.), hypertension and diabetes, history of thoracic surgery (esophageal, pulmonary, cardiac surgery or surgery of rib fracture) and smoking history (past or current smoker or never smoker).
Resection margin distance was defined as the distance from tumor to the closest stapled resection margin. The tumor size, which was used to evaluate the quality of resection margin distance, and margin distance were evaluated and recorded by pathologists. During margin distance measurement, tumor was transected, and its perimeter was delineated. Then, the distance from tumor to the cutting edge was measured. Tumor’s distance to pleura and the tumor size, which were used for risk evaluation and predictive model construction, were evaluated based on the preoperative CT examination. Thoracic surgeons with over 5 years of clinical experience viewed the preoperative chest CT images and measured the distance from tumor to the nearest pleura for each patient.
Principles of surgical therapy stated in the NCCN Guidelines of NSCLC mentioned that wedge resection should achieve parenchymal resection margins ≥2 cm or the size of the nodule (8). Thus, guideline discordant wedge resection margin in our study was defined when the ratio of resection margin distance to tumor size was <1 and guideline concordant resection margin was defined when the ratio was ≥1.
Statistical analysis
Based on the quality of wedge resection margin, patients were divided into two groups (patients with guideline discordant margin and with guideline concordant margin). Student’s t-test or Wilcoxon test was used to test continuous variables expressed as mean (standard deviation) or median (interquartile range). The Chi-squared test was applied for comparing categorical variables, reported as frequencies (ratio).
The nomogram was developed as follows: First, univariable logistic regression analysis was used to evaluate the ability of each variable in predicting the risk of guideline discordant wedge resection margin. Second, those variables with P values <0.20 and clear clinical correlation with wedge resection margin were included in the multivariable logistic regression analysis. Based on the multivariable logistic regression results, a nomogram was built using the R package “rms”.
A P value <0.05 was considered significant. All analyses were conducted by R software (version 4.1.1, R Foundation for Statistical Computing, Vienna, Austria).
Measurement of performance and validation
Data from 180 patients who received pulmonary wedge resection between March 2023 and January 2024 in the Department of Thoracic Surgery, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine were retrospectively collected as the internal validation data set. We used the concordance index (C-index) and receiver operating characteristic (ROC) curve to evaluate the accuracy of the predictive model in either data development or internal validation data set (12). The optimal cutoff value was determined based on ROC analysis. A Hosmer-Lemeshow test was applied for an indication of goodness of fit between the predicted and observed risks. The calibration curve visualized the discrimination between the predicted and actual risk of guideline discordant wedge resection. Decision curve analysis was finally used to evaluate the net benefit which indicated the clinical utility of the model, by using the R package “rmda”.
Results
Patient characteristics
Between April 2014 and February 2023, a total of 932 patients had received a lung wedge resection at Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. Patients with missing information or postoperative pathology that revealed metastases or benign tumors were ruled out. Another 34 patients with pulmonary lesions more than 2 cm in diameter according to preoperative CT examination were also excluded. Finally, 530 patients were included for analysis. The majority (70.4%, 373/530) of patients were female and 29.6% (157/530) were male. The age range of the patients was 20 to 89 years with a median age of 56 years. Most of the enrolled patients underwent minimally invasive surgery, 87.2% (462/530) patients received video-assisted thoracic surgery, 9.8% (52/530) received robotic-assisted surgery, and only 3.0% (16/530) underwent thoracotomy. A total of 48 (9.1%) patients received simultaneous wedge resection combined with lobectomy, or segmentectomy for multiple primary lung tumors. According to the requirement for wedge resection margin in the NCCN guideline, 62.8% of the surgeries (333/530) were defined as guideline concordant and 37.2% (197/530) were guideline discordant. Patients were divided into guideline concordant group or discordant group. The characteristics of patients in the two groups are listed in Table 1.
Table 1
| Characteristic | Patients with discordant margin (n=197) | Patients with concordant margin (n=333) | P |
|---|---|---|---|
| Sex, n (%) | 0.79 | ||
| Male | 57 (28.9) | 100 (30.0) | |
| Female | 140 (71.1) | 233 (70.0) | |
| Age (years), median [IQR] | 62.0 [19.0] | 54.0 [18.0] | <0.001 |
| ≥20 to <50, n (%) | 42 (21.3) | 120 (36.0) | <0.001 |
| ≥50 to <70, n (%) | 104 (52.8) | 189 (56.8) | |
| ≥70, n (%) | 51 (25.9) | 24 (7.2) | |
| BMI (kg/m2), median [IQR] | 23.80 [4.00] | 21.74 [2.59] | <0.001 |
| %FEV1, median [IQR] | 0.98 [0.22] | 0.98 [0.22] | <0.001 |
| ≥0.8, n (%) | 143 (72.6) | 286 (85.9) | 0.001 |
| 0.5 to <0.8, n (%) | 51 (25.9) | 43 (12.9) | |
| <0.5, n (%) | 3 (1.5) | 4 (1.2) | |
| FEV1/FVC, median [IQR] | 0.82 [0.14] | 0.89 [0.13] | <0.001 |
| ≥0.7, n (%) | 171 (86.8) | 323 (97.0) | <0.001 |
| <0.7, n (%) | 26 (13.2) | 10 (3.0) | |
| %MVV, mean (SD) | 0.81 (0.21) | 0.88 (0.20) | <0.001 |
| Minimal distance to pleura [cm], median [IQR] | 0.45 [0.90] | 0.35 [0.79] | 0.48 |
| Max distance to pleura [cm], median [IQR] | 1.66 [0.80] | 1.33 [0.86] | <0.001 |
| Tumor size [cm], median [IQR] | 1.10 [0.61] | 0.85 [0.43] | <0.001 |
| Margin distance [cm], median [IQR] | 0.60 [0.50] | 1.50 [1.00] | <0.001 |
| Surgical type, n (%) | 0.50 | ||
| Wedge resection | 177 (89.8) | 305 (91.6) | |
| Wedge resection + lobectomy/segmentectomy | 20 (10.2) | 28 (8.4) | |
| Surgical technology, n (%) | 0.23 | ||
| Thoracotomy | 6 (3.0) | 10 (3.0) | |
| VATS | 166 (84.3) | 296 (88.9) | |
| RATS | 25 (12.7) | 27 (8.1) | |
| Upper lobe surgery, n (%) | 0.52 | ||
| Yes | 132 (67.0) | 214 (64.3) | |
| No | 65 (33.0) | 119 (35.7) | |
| Location of surgery, n (%) | 0.08 | ||
| Left | 91 (46.2) | 128 (38.4) | |
| Right | 106 (53.8) | 205 (61.6) | |
| Preoperative localization, n (%) | <0.001 | ||
| Yes | 110 (55.8) | 252 (75.7) | |
| No | 87 (44.2) | 81 (24.3) | |
| Diabetes, n (%) | <0.001 | ||
| Yes | 37 (18.8) | 19 (5.7) | |
| No | 160 (81.2) | 314 (94.3) | |
| Hypertension, n (%) | 0.31 | ||
| Yes | 57 (28.9) | 83 (24.9) | |
| No | 140 (71.1) | 250 (75.1) | |
| Disease of respiratory system, n (%) | 0.10 | ||
| Yes | 10 (5.1) | 8 (2.4) | |
| No | 187 (94.9) | 325 (97.6) | |
| Cardiovascular disease, n (%) | 0.70 | ||
| Yes | 16 (8.1) | 24 (7.2) | |
| No | 181 (91.9) | 309 (92.8) | |
| Smoking, n (%) | 0.40 | ||
| Yes | 30 (15.2) | 42 (12.6) | |
| No | 167 (84.8) | 291 (87.4) | |
| History of thoracic surgery, n (%) | 0.81 | ||
| Yes | 19 (9.6) | 30 (9.0) | |
| No | 178 (90.4) | 303 (91.0) |
IQR, interquartile range; BMI, body mass index; %FEV1, percent forced expiratory volume in one second; FEV1/FVC, the ratio of forced expiratory volume in one second and forced vital capacity; %MVV, percent maximal voluntary ventilation; SD, standard deviation; VATS, video-assisted thoracic surgery; RATS, robotic-assisted thoracic surgery.
Risk factors of guideline discordant wedge resection
To explore the factors affecting the quality of wedge resection margin for patients, we first performed univariable statistical analysis for each factor (Table 1). The result indicated that the quality of resection margin was related to age distribution and BMI (P<0.001). Patients with higher age and BMI tended to have guideline discordant resection margin. Of patients aged ≥70 years, 51 wedge resection were guideline discordant, while 24 were concordant. History of diabetes also correlated with lower incidence of guideline concordant surgical margin (P<0.001). Furthermore, pulmonary ventilation function (%FEV1, FEV1/FVC and %MVV, P<0.001), tumor’s max distance to pleura (P<0.001), tumor size (P<0.001) and surgical margin (P<0.001) were also found to be significantly associated with the quality of wedge resection within the variables considered. Among all patients included, patients with guideline discordant resection margin had a median tumor’s max distance to pleura of 1.66 cm, median tumor size of 1.10 cm and median surgical margin of 0.60 cm, whereas those with guideline concordant margin were 1.33, 0.85, and 1.50 cm respectively. Preoperative CT-guided pulmonary nodule localization is also significantly associated with quality of margin. Most of the patients with preoperative localization had guideline concordant margin (252/362, 69.6%), while 48.2% (81/168) patients without preoperative localization were guideline concordant (Table 1).
Then, the univariable logistic regression analysis showed that a guideline discordant resection margin was associated with age [odds ratio (OR): 1.054, P<0.001], BMI (OR: 1.148, P<0.001), pulmonary function (%FEV1, FEV1/FVC and %MVV, P<0.001), tumor’s max distance to pleura (OR: 1.752, P<0.001), tumor size (OR: 6.473, P<0.001), preoperative localization (OR: 0.406, P<0.001) and history of diabetes (OR: 3.822, P<0.001) (Table 2). Patients, who were older, had a larger tumor, and a longer distance from the pleura to pulmonary lesions were more likely to receive guideline discordant wedge resections. And those with higher BMI, history of diabetes and worse ventilation pulmonary function also had higher risk of discordant resection margin. Meanwhile, right side surgery (OR: 0.727, P=0.08) and preoperative localization seemed to ensure a safe resection margin.
Table 2
| Variable | OR (95% CI) | P |
|---|---|---|
| Sex, female vs. male | 1.054 (0.716–1.552) | 0.79 |
| Age (years) | 1.054 (1.038–1.071) | <0.001 |
| BMI (kg/m2) | 1.148 (1.079–1.222) | <0.001 |
| %FEV1 | 0.145 (0.053–0.394) | <0.001 |
| 0.5≤ %FEV1 <0.8 vs. %FEV1 ≥0.8 | 2.309 (1.466–3.637) | <0.001 |
| %FEV1 <0.5 vs. %FEV1 ≥0.8 | 1.490 (0.329–6.745) | 0.61 |
| FEV1/FVC | 0.002 (0.002–0.010) | <0.001 |
| <0.7 vs. ≥0.7 | 4.695 (2.204–10.002) | <0.001 |
| %MVV | 0.173 (0.071–0.422) | <0.001 |
| Minimal distance to pleura (cm) | 1.044 (0.770–1.417) | 0.78 |
| Max distance to pleura (cm) | 1.752 (1.343–2.285) | <0.001 |
| Tumor size (cm) | 6.473 (3.871–10.825) | <0.001 |
| Margin distance (cm) | 0.013 (0.006–0.028) | <0.001 |
| Surgical type, wedge resection + lobectomy/segmentectomy vs. wedge resection | 1.231 (0.673–2.249) | 0.50 |
| Surgical technology | ||
| VATS vs. thoracotomy | 0.935 (0.334–2.618) | 0.90 |
| RATS vs. thoracotomy | 1.543 (0.489–4.869) | 0.46 |
| Upper lobe surgery, yes vs. no | 1.129 (0.778–1.638) | 0.52 |
| Location of surgery, right vs. left | 0.727 (0.509–1.039) | 0.08 |
| Preoperative localization, yes vs. no | 0.406 (0.279–0.592) | <0.001 |
| Diabetes, yes vs. no | 3.822 (2.129–6.860) | <0.001 |
| Hypertension, yes vs. no | 1.226 (0.826–1.821) | 0.31 |
| Disease of respiratory system, yes vs. no | 2.172 (0.843–5.600) | 0.11 |
| Cardiovascular disease, yes vs. no | 1.138 (0.589–2.199) | 0.70 |
| Smoking status, past or current smoker vs. never smoker | 1.245 (0.751–2.064) | 0.40 |
| History of thoracic surgery, yes vs. no | 1.078 (0.589–1.972) | 0.81 |
OR, odds ratio; CI, confidence interval; BMI, body mass index; %FEV1, percent forced expiratory volume in one second; FEV1/FVC, the ratio of forced expiratory volume in one second and forced vital capacity; %MVV, percent maximal voluntary ventilation; VATS, video-assisted thoracic surgery; RATS, robotic-assisted thoracic surgery.
Multivariable logistic regression analysis
Factors were included in the multivariable model if P<0.05 in the univariable analysis and those clinically meaningful factors with P<0.20 were also considered. According to the definition in the NCCN guideline, the surgical margin was considered directly associated with quality of wedge resection margin and was excluded from the multivariable analysis. Patients’ baseline characteristics, including sex, age, BMI, pulmonary ventilation function, comorbidities, history of thoracic surgery and smoking history, were considered to have no direct technical correlation with wedge resection margin and were also excluded.
Multivariable logistic regression analysis showed that tumor size (OR: 4.391, P<0.001), preoperative localization (yes vs. no, OR: 0.535, P=0.003) and surgical location (right vs. left, OR: 0.630, P=0.02) were significantly correlated with guideline discordant wedge resection (Figure 1, Table 3). Increased tumor’s max distance to pleura is commonly considered to greatly increase depth of resection range and complexity of surgery, which may affect the achievement of the guideline concordant surgical margin. Thus, tumor’s max distance to pleura could be clinically related to resection margin and was included in the following model development, although there was only marginally significant correlation with the quality of wedge resection margin in multivariable analysis (OR: 1.337, P=0.06).
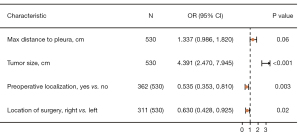
Table 3
| Factor | Coefficient | SE | OR (95% CI) | P |
|---|---|---|---|---|
| Max distance to pleura (cm) | 0.290 | 0.208 | 1.337 (0.986–1.820) | 0.06 |
| Tumor size (cm) | 1.480 | 1.307 | 4.391 (2.470–7.945) | <0.001 |
| Preoperative localization, yes vs. no | −0.626 | 0.113 | 0.535 (0.353–0.810) | 0.003 |
| Location of surgery, right vs. left | −0.462 | 0.124 | 0.630 (0.428–0.925) | 0.02 |
| Constant | −1.847 | 0.061 | 0.158 (0.074–0.336) | <0.001 |
SE, standard error; OR, odds ratio; CI, confidence interval.
Development and validation of a predictive nomogram
The four parameters mentioned above (tumor’s max distance to pleura, tumor size, location of surgery and preoperative localization) were incorporated to develop a nomogram for predicating the risk of guideline discordant wedge resection margin (Figure 2). C-index of the model was 0.720 and ROC curve similarly showed that the model has good discrimination with the best cut-off value of 0.393 (specificity =0.739, sensitivity =0.599) (Figure 3A, Table 4). The C-index for internal validation was 0.761. The calibration plot was shown in Figure 3B, indicating a close agreement between the predicted and actual risk of guideline discordant wedge resection. The Hosmer-Lemeshow goodness-of-fit test was nonsignificant for both data development (P=0.70) and validation data set (P=0.45), indicating good model for the data. A decision curve analysis curve was performed to ascertain the clinical usefulness of the nomogram. The result showed good clinical application in predicting the risk of guideline discordant wedge resection due to wide ranges of threshold probabilities (about 0.10–0.90) (Figure 3C). Moreover, the predicted probability of guideline discordant wedge resection margin matched closely with the actual frequency in the validation cohort (Table 5).
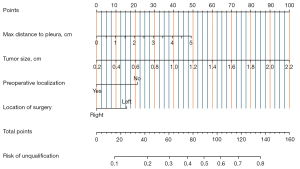
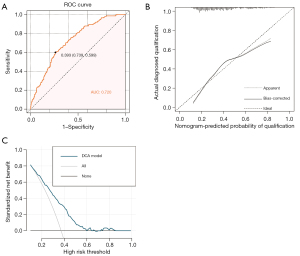
Table 4
| Aspect | Measure | Development data set | Validation data set |
|---|---|---|---|
| Discrimination | C-index | 0.720 | 0.761 |
| Goodness-of-fit test | Hosmer-Lemeshow, P | 0.70 | 0.45 |
C-index, concordance index.
Table 5
| Estimated risk | Incidence of guideline discordant wedge resection (n) | Frequency of guideline discordant wedge resection (%) |
|---|---|---|
| 0–15% | 3 | 10.3 |
| >15–30% | 10 | 18.2 |
| >30–45% | 16 | 36.4 |
| >45% | 30 | 57.7 |
Discussion
Wedge resection is one of the most widely used type of lung resection, especially for early-stage NSCLC (5,13,14). As reported in previous publications, a guideline concordant wedge resection margin of more than 2 cm or greater than the diameter of the pulmonary lesion should be essential for the best patient survival after surgery (9-11,15). According to a multicenter, prospective study, which analyzed the margin status of 118 NSCLC cases of wedge resection, maximum tumor diameter and margin distance were independent factors of predictive malignant positive margin after wedge resection. A margin distance greater than the maximum tumor diameter guaranteed a negative margin (9). Mohiuddin et al. investigated the risk of local recurrence after wedge resection based on data of 479 NSCLC cases, and concluded that an increased margin distance was significantly associated with a lower risk of local recurrence (11).
Even though, an adequate resection margin is significantly associated with lack of tumor recurrence, and has been required in NCCN guideline (7,8), a portion of patients still underwent wedge resection with an insufficient margin distance. According to the study of Mohiuddin et al., 61.0% of cases had wedge resection margins of less than or equal to 10 mm, whereas, only 24.6% of tumors had diameters of 1 to 10 mm. Accordingly, the incidence of guideline discordant resection margin could be at least 36.4% (11). An earlier study also reported that, the average wedge resection margin distance of 9.2 mm was achieved for 118 cases whose tumors had an average diameter of 15.3 mm (9). Our study also reported 37.2% cases of wedge resection which did not achieve sufficient resection margin. Therefore, the quality of resection margin should be seriously considered during the design of surgical plan and surgery. Given that no previous study has reported the risk of an adequate resection margin, we innovatively evaluated the independent risk factors for a guideline discordant wedge resection margin and developed a clinical model to preoperatively predict the risk of for individual patients in this study. Based on the model, which contains four parameters (max distance to pleura, tumor size, tumor location and preoperative localization), the quality of resection margin can be accurately predicted. The associated nomogram enables the visualization of our model and could easily be integrated into clinical practice.
According to our univariable analysis, age and BMI were demonstrated to be one of the risk factors for a guideline discordant resection margin. The plausible explanation could be that age and BMI are key factors impacting patients’ general condition. Older patients with higher BMI are expected to have poorer pulmonary function, performance status and more serious concomitant disease. In these cases, surgeons might unintentionally prefer more conservative treatment strategies, and therefore, result in guideline discordant resection margin. Poorer pulmonary function or history of diabetes are also related to delayed rehabilitation and relatively poorer quality of life after surgery (16-19), and could also have impact on surgeons’ decision-making during surgery. However, there is no direct technical correlation between factors related to quality of life and the quality of wedge resection margin. Factors such as age and pulmonary function cannot technically impact the difficulty and complexity of surgery. Therefore, we excluded these factors from the subsequent multivariable regression. Only those with clear clinical relevance were included as candidates in multivariable analysis.
Our univariable and multivariable analyses revealed that tumor size and max distance between tumor and pleura are significant risk factors of guideline discordant resection margin. According to NCCN guideline, an increased tumor size is associated with the need for a longer resection margin (8). The distance between the tumor and the pleura has an important impact on the volume of pulmonary tissue resected during wedge resection and increases the complexity of the surgery. According to our model, the risk of a guideline discordant margin significantly increased for pulmonary lesions having a diameter higher than 1 cm or a max distance to pleura more than 3 cm. Consequently, an optimized surgical plan of wedge resection should be made for large or deep pulmonary tumors to ensure the radical resection of the tumor. Segmentectomy or lobectomy should also be considered under this circumstance.
Preoperative CT-guided hook-wire localization is widely used in our department, especially for small pulmonary nodules with higher distance to pleura. In this case series, 68.3% (362/530) patients received preoperative localization before wedge resection. The guideline concordant margin rate was 69.6% after preoperative localization, which was significantly higher than those without localization (48.2%). Theoretically, preoperative localization can provide more accurate tumor location information, thus assisting surgeons in designing refined and compliant resection plans to reduce unnecessary resection range while achieving a reasonable margin.
In our department, intraoperative macroscopic evaluation of tumor margin was regularly conducted by surgeons after the resection of pulmonary tumor and the associated lung tissue. If margin distance was considered inadequate by surgeons during surgery, a re-resection would be carried out to ensure a more optimal margin. Even though intraoperative evaluation was performed in our study, a portion of cases still experienced guideline discordant resection margin. The potential explanations could be that the visual and macroscopic evaluation was relatively inaccurate compared with pathological evaluation. Meanwhile, the resected specimen was deflated and experienced shrinkage after formalin fixation (20), which may result in decreased resection margin. Given all that, even after the visual confirmation of a safe margin distance during surgery, the resection margin could still be insufficient. For those patients with high risk of insufficient margin, preoperative nodule localization or individualized surgical plans should be made, instead of relying on the experience of surgeon.
This preoperative predictive model of margin quality has several limitations. First, an external validation will be needed to further evaluate the generalization of our model in a multicenter setting. Postoperative long-term follow-up will also be necessary to confirm the clinical significance of guideline discordant margin. In addition, confounding factors may exist due to the retrospective nature of this study. Moreover, the predictive model and the associated nomogram are relatively complex, and not always easy to apply when facing possible intraoperative change of surgical plan. Despite the above limitations, this model could accurately and efficiently identify patients with higher risk of guideline discordant wedge resection. An optimized surgical plan or preoperative nodule localization could therefore be made to ensure the radical resection of malignancy.
Conclusions
In conclusion, we have developed a preoperative predictive model to estimate the risk of a guideline discordant wedge resection margin for individual patient. Optimized and individualized surgical plans or preoperative nodule localization can be made for high-risk patients.
Acknowledgments
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the TRIPOD reporting checklist. Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-22/rc
Data Sharing Statement: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-22/dss
Peer Review File: Available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-22/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tlcr.amegroups.com/article/view/10.21037/tlcr-24-22/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine (approval number 2023-15) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Leiter A, Veluswamy RR, Wisnivesky JP. The global burden of lung cancer: current status and future trends. Nat Rev Clin Oncol 2023;20:624-39. [Crossref] [PubMed]
- O'Dowd EL, Tietzova I, Bartlett E, et al. ERS/ESTS/ESTRO/ESR/ESTI/EFOMP statement on management of incidental findings from low dose CT screening for lung cancer. Eur Respir J 2023;62:2300533. [Crossref] [PubMed]
- Saji H, Okada M, Tsuboi M, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022;399:1607-17. [Crossref] [PubMed]
- Altorki NK, Wang X, Wigle D, et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet Respir Med 2018;6:915-24. [Crossref] [PubMed]
- Altorki N, Wang X, Kozono D, et al. Lobar or Sublobar Resection for Peripheral Stage IA Non-Small-Cell Lung Cancer. N Engl J Med 2023;388:489-98. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. NCCN Guidelines® Insights: Non-Small Cell Lung Cancer, Version 2.2023. J Natl Compr Canc Netw 2023;21:340-50. [Crossref] [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2022;20:497-530. [Crossref] [PubMed]
- Sawabata N, Ohta M, Matsumura A, et al. Optimal distance of malignant negative margin in excision of nonsmall cell lung cancer: a multicenter prospective study. Ann Thorac Surg 2004;77:415-20. [Crossref] [PubMed]
- El-Sherif A, Fernando HC, Santos R, et al. Margin and local recurrence after sublobar resection of non-small cell lung cancer. Ann Surg Oncol 2007;14:2400-5. [Crossref] [PubMed]
- Mohiuddin K, Haneuse S, Sofer T, et al. Relationship between margin distance and local recurrence among patients undergoing wedge resection for small (≤2 cm) non-small cell lung cancer. J Thorac Cardiovasc Surg 2014;147:1169-75; discussion 1175-7. [Crossref] [PubMed]
- Robin X, Turck N, Hainard A, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 2011;12:77. [Crossref] [PubMed]
- Shi Y, Wu S, Ma S, et al. Comparison Between Wedge Resection and Lobectomy/Segmentectomy for Early-Stage Non-small Cell Lung Cancer: A Bayesian Meta-analysis and Systematic Review. Ann Surg Oncol 2022;29:1868-79. [Crossref] [PubMed]
- Kneuertz PJ, Abdel-Rasoul M, D'Souza DM, et al. Wedge Resection vs Lobectomy for Clinical Stage IA Non-Small Cell Lung Cancer With Occult Lymph Node Disease. Ann Thorac Surg 2023;115:1344-51. [Crossref] [PubMed]
- Moon Y, Park JK, Lee KY, et al. Prognosis after wedge resection in patients with 8(th) edition TNM stage IA1 and IA2 non-small cell lung cancer. J Thorac Dis 2019;11:2361-72. [Crossref] [PubMed]
- Choi S, Park J. Surgical outcomes and prognosis of non-small-cell lung cancer in patients with chronic lung diseases: a retrospective analysis. Eur J Cardiothorac Surg 2020;58:357-64. [Crossref] [PubMed]
- Roy E, Rheault J, Pigeon MA, et al. Lung cancer resection and postoperative outcomes in COPD: A single-center experience. Chron Respir Dis 2020;17:1479973120925430. [Crossref] [PubMed]
- Kaseda K, Hishida T, Masai K, et al. Clinicopathological and prognostic features of operable non-small cell lung cancer patients with diabetes mellitus. J Surg Oncol 2021;123:332-41. [Crossref] [PubMed]
- Lejeune D, Hardy PY, Kaba A, et al. Postoperative morbidity and mortality in patients with diabetes after colorectal surgery with an enhanced recovery program: A monocentric retrospective study. J Visc Surg 2023;160:180-7. [Crossref] [PubMed]
- Lam D, Kaneko Y, Scarlett A, et al. The Effect of Formalin Fixation on Resection Margins in Colorectal Cancer. Int J Surg Pathol 2019;27:700-5. [Crossref] [PubMed]


